A Framework to Research the Social Determinants of ICTs for E-Health
Lareen Newman, Senior Research Fellow,
Southgate Institute for Health Society & Equity,
Flinders University, Adelaide, South Australia. Email:
[email protected]
Francisco
Lupiáñez-Villanueva, Associate
Professor, Information and Communication Sciences
Department, Applied Social Science and Behavioral
Economics Research Group, Universitat Oberta de
Catalunya, Barcelona, Spain. Email: [email protected]
INTRODUCTION
This article discusses the challenges of combining significantly different methodological approaches to investigate citizens' access to e-health. We define the term access beyond broadband connectivity (material access), to also include motivation, skills and different type of usages (van Dijk, 2005), which in e-health ranges from accessing online healthcare information, services and clinical treatment, to self-support. Around the globe, e-health has continued to expand with the expectations that it will both reduce healthcare expenditure and improve quality and access to healthcare for all citizens (Griffiths et al 2006). However, emerging evidence suggests that, if not managed carefully, e-health will further exacerbate health inequities because those with poorer health are often those with lower or no information and communication (ICT) use (Espanha & Lupiáñez-Villanueva 2009; Newman et al 2012).
To date, e-health research in developed countries has focused on clinical and health systems, on health professionals' and institutions' ability to move their services online, and on describing the types of health issues which can be addressed when citizens connect with e-health. Less attention has been paid to understanding the socio-demographic factors shaping citizens' ICT use/non-use in terms of how this impacts on their ability to uptake e-health opportunities (some exceptions are van Deursen & van Dijk 2011; Lockwood et al 2013; Newman et al 2012; and Wen et al 2011). This is despite the fact that citizens' capability to interact with health systems online has long been a barrier to e-health uptake (see eg Eysenbach 2001). In Australia, for example, the National E-Health Strategy and National E-Mental Health Strategy simply 'encourage' consumers to engage in e-health without any consideration of their ICT status (Australian Health Ministers Advisory Council 2008; Department of Health & Ageing 2010).
What requires urgent attention is therefore investigating how the digital divide plays out in e-health, in relation to investigating the resources which different citizen groups require for ICT access and how this in turn shapes whether or not they can access the potential benefits of using the Internet for health purposes. This paper outlines two different methodological approaches to investigating this and argues that, despite methodological challenges to bringing them together, doing so can go some way to addressing the gap in knowledge: positivist methodologies which use quantitative research methods in the research field of Information & Communication Science, and critical theory approaches which use qualitative research methods in Public Health.
METHODOLOGICAL APPROACHES
A Positivist Approach to Understand E-health Access
Our large scale quantitative surveys conducted across the European Union have investigated citizens' ICT use for e-health (access for health purposes such as looking for health information or contacting a doctor). The largest involved surveying 14,000 people in 14 countries (Lupiáñez, Maghiros & Abadie 2013). It produced information about the patterns of ICT use guided by the positivist paradigm. It collected self-reported indicators divided into five different blocks of questions: (1) Health status and health care and social care services use; (2) Health attitude and health information sources; (3) Internet and ICT uses; (4) Health related use of ICTs and the Internet; and (5) Socio-demographic profile of participants. Even though the survey was conducted only with Internet users, the results reveal that new health inequities are emerging as these overlap with the different manifestations of the divide which are also determinants of ICT use(see Table 1 extracted from Peña-López, 2009). For example, individuals aged between 55-74 who are healthy are more likely to use ICTs for Health than individuals with worse health status. On the contrary, individuals aged between 16-54 with chronic conditions, going under long-term treatment and with more than one health problem are more likely to use ICTs for Health than individuals without these type of health problems (Lupiáñez, Maghiros & Abadie 2013). These emerging health inequities could be considered, especially for the elderly, as a new expression of the inverse care law (Tudor Hart 1971): an "inverse care law 2.0".
Source: Extracted from Peña-Lopez 2009 p.88
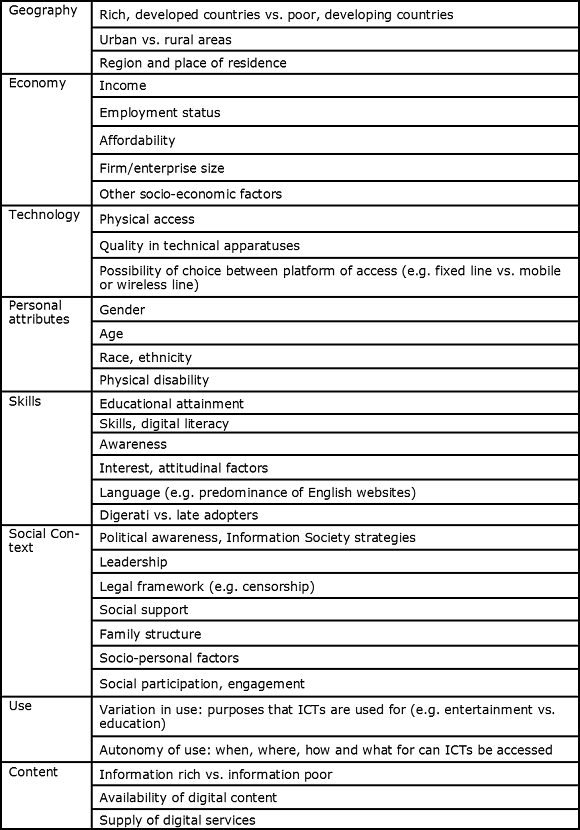
A strength of this quantitative approach is that it provides data from a large number of randomly selected individuals from which generalized inferences can be made about the phenomena under study. In this context, ICT access was examined in a broad sense to identify what variables related to the digital divide were related to e-health access. It is worth pointing out that the concept of ICT access in this study nevertheless was limited simply to measuring whether or not citizens had or did not have physical access to the Internet and relevant devices.
A weakness of this approach is that, methodologically, it cannot explain the 'why' - why do we see these data patterns and what are their causes. The digital divide literature suggests that there are social, economic, and cultural factors influencing why individuals or certain population groups have (or do not have) the Internet or device access in the first place (eg van Dijk 2005) but we know little about how this in turn enables them to have (or prevents them having) access to e-health (ie how the digital divide interacts with e-health access). Nevertheless, as has been reported elsewhere (O'Neill et al, 2014), online surveys cause selection bias because they exclude those who do not have Internet access or adequate digital skills. Another strength of the above approach is that it reveals the multidisciplinary scope of the digital divide that can be approached from different disciplines such as Economics, Geography, Psychology, Sociology, Informatics, Social Public Health and Pedagogy, as well as through the different methods used by those disciplines. In this regard, the digital divide as an individual and social phenomenon is being researched using social science as an umbrella beyond a specific discipline.
A Critical Theory Approach to the Digital Divide
Within public health, a critical theory methodology or critical perspective (Crotty 1998) encourages inquiry into what drives power structures and the unequal distribution of resources across a population, because these impact on our opportunities for health and hence on unfair and remediable differences (inequities) in health status and health outcomes. Since these 'inequities' are not a given but are structurally determined, they are unfair, avoidable and remediable (Dahlgren & Whitehead 1991), which introduces a moral and ethical dimension to research in this field. A social gradient in health has been recognised, whereby those nearer the top of the socioeconomic spectrum have better health than those further down, and applying this concept from the health field to digital research suggests there is a similar "digital gradient" (Newman et al 2010). This approach lends itself to in-depth qualitative research that can ask individuals their perception of why various aspects of their socioeconomic and geographic position may be influencing their ICT use (e.g. Newman, Biedrzycki & Baum 2009) and in turn how this influences their access to healthcare (e.g. Baum et al 2012). Critical information systems research has also drawn on this methodology to 'turn the spotlight' onto issues of web (in)accessibility for particular disadvantaged groups such as people with disabilities (Adam & Kreps 2006) and Walsham (2012) has recently argued the need to reinvigorate this ethical aspect of ICT research so that we can 'make a better world'.
In Australia there has been little in-depth qualitative research into ICT use and into barriers/facilitators of ICT use among disadvantaged groups and the knock-on impact to ICTs for Health purposes, although recent research has filled this gap (Baum et al 2012; Newman et al 2012).The focus was on exploring citizens' perspectives on the best ways to enable their access and use of computers, the Internet and mobile phones to overcome the digital divide and to access e-health. Interviews and focus groups identified a wide variety of reasons for unequal ICT use among lower income and disadvantaged groups, well beyond differences in ICT ownership and ICT skills (Newman et al 2010). The data was also analysed by applying Bourdieu's Theories of Capitals (Bourdieu 1977, 1986), which sit predominantly in the field of sociology and allow a critical investigation of the social reproduction of inequities in ICT use. While Helsper (2012) has applied this thinking to shape quantitative variables for ICT use research, we drew on this approach using qualitative research to uncover the resources ('capitals') which underlie ICT access and use but which are queried less often than ICT skills and digital literacy. For adults, our in-depth qualitative research shows that these resources include basic reading ability and living in a social group who will not steal digital devices (Baum et al 2012). For young people who are born with physical disabilities or acquire a brain injury these resources include having a family who is ICT-competent and a family who are aware of and can afford to purchase disability-assistive technologies which enable ICT use (Newman, Browne-Yung, et al in press). A benefit of this research methodology is that it values the subjective views ('voices') of participants and hence usually involves in-depth face-to-face interviews, meaning that it can collect data from those who do not have Internet access or adequate digital skills (or who are simply not interested or willing) to respond to online surveys. Many of the underlying resources fall into the categories listed in Table 1, suggesting the applicability of the well-known Social Determinants of Health Framework.
TOWARDS A "SOCIAL DETERMINANTS OF ICTS FOR HEALTH" FRAMEWORK
We argue that what is needed to guide further research on the digital divide's impact on e-health access is a framework which allows us to collect and analyse data that combines the two methodological approaches, each informing the other, and which can identify both the quantitative relationships between and the qualitative explanations for ICT use and e-health access ie ICTs for Health. We see that a framework which could guide a research combination of these two methodological approaches would categorise factors at each level that shapes citizens' ability to benefit from e-health, provide explanations for the causes of the patterns and interrelationships between them, and enable a critical-perspective revelation of unjust and remediable differences between different population groups, and particularly among disadvantaged groups. If we can identify both factors and relationships, then health policymakers and practitioners will be better informed as to how to increase support for citizens to access to e-health. Such factors might include providing individuals with funds to purchase ICT devices or connections to enable searching on a website for health information. At the same time, broader factors influence both ICT use and opportunities for health, including national policies on telecommunications infrastructure and broadband speeds, and at the community level the provision of free and easy-to-reach public Internet access. These broader influences are known in the global health literature as the social determinants of health, which has become widely influential since the World Health Organisation's focused Commission on the Social Determinants of Health (2008).
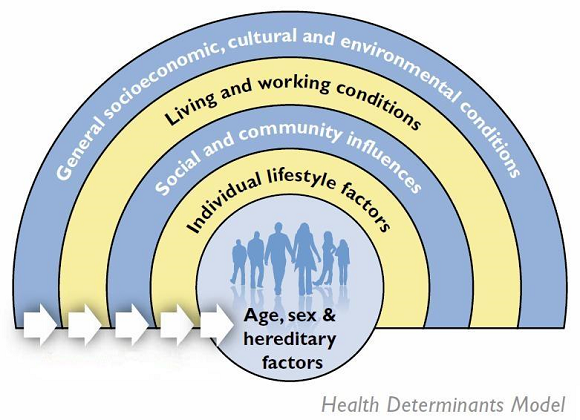
The World Health Organisation (1986) has long recognised that people's opportunities to lead healthy lives are shaped by policies and institutional practices. In the early 1990s, Dahlgren and Whitehead (1991) set out a strategic approach to promote greater equity in health between different population groups in Europe by highlighting the different levels of society which policy could target in order achieve change. This is shown diagrammatically in Figure 1. This approach moves the focus from only trying to change individual behaviours to also addressing the broader contexts which shape that behaviour ie an individual's family and community context, the opportunities available in terms of what is provided by various levels of government and private sector (infrastructure, employment, welfare, education, etc), plus forces at the societal level such as cultural norms and global level forces such as international trade, treaties, governance, and globalisation.
Source: www.health-inequalities.eu (based on Dahlgren & Whitehead 1991).
GOING FORWARD
A tested version of the "Social Determinants of ICTs for Health Framework" does not yet exist but, based on earlier research, the version below in Figure 2 has been developed. We believe this is an innovative approach that can bring together our two areas of research to provide a comprehensive investigation of factors which shape the impacts of the digital divide in ICT access/use on citizens' access to e-health. We will be developing and refining the Framework to guide our combined future work as we believe that this will ensure that key underlying factors specific to understanding the digital divide in e-health access are not overlooked. We find that this can particularly occur in developed countries due to the assumption that "everyone is online" (via the Internet and/or on mobile devices), yet data continue to show that even if every citizen in a population has technical access, all users are not created equal and their devices will function and be used at a wide range of levels, from basic to very advanced, which in itself still results in a "digital gradient".
Figure 2 shows that social determinants of health and health inequities, therefore structural and intermediary determinants, produce different levels of ICT access (motivation, material, skills and usage). This unequal access to ICT will generate different levels of ICT for Health access as well as different levels of willingness to use ICT for Health. In addition, ICT for Health access depends on the properties of ICT and the relationship between Motivation, ICT for Health readiness and Internet Health information. In this regard, Motivation includes Triggers, Empowerment and Barriers; ICT for Health readiness includes Awareness, Material access; Skills and Usage and Internet Health information includes how individuals use and evaluate this type of information for themselves or for others (social life of information) as well as their perception about usefulness and learning. Lastly, ICT for Health Access gives rise to different level of Participatory Health through the utilisation of health information (individual and social uses) and behavioural changes causes by how ICT for Health impact on: Health management; Health care demand and Health care quality. These impacts could modify both structural and intermediary determinants and the distribution of health and well-being.
Source: Lupiáñez F, Maghiros I, Abadie F (2013).
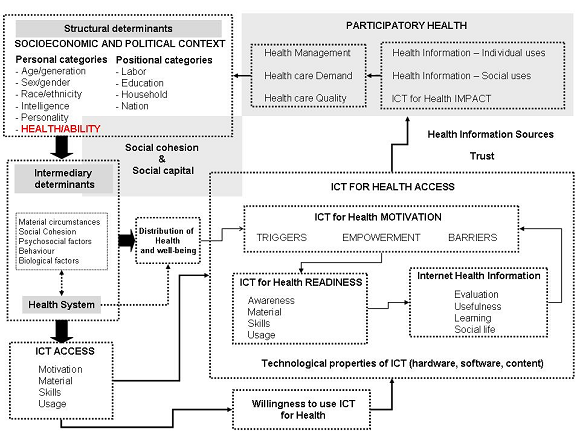
We intend that the Framework will allow us to pinpoint the key social determinants layers, including those political and policy layers which strongly influence the distribution of digital infrastructure, other resources, health and wellbeing etc, as well as identifying other sub-areas relevant to ICT use and healthcare access. We intend that the Framework will guide identification of key factors that can be investigated by both quantitative variables (the prevalence, frequency, quality of ICT use and Healthcare access) and qualitative data (the reasons for these differences, motivational issues and social contexts, and what different population groups believe underpin resource differentials). From this we will then have better knowledge of key points of entry for action by services and policymakers to improve citizens' ICT Use for Health.
In the first instance, our plans are to apply the framework to inform two pieces of work:
- A project with a broader group of researchers to investigate e-inclusion and e-health access for citizens and how these can be addressed at the various levels of the Social Determinants by health services and health policymakers though changing the ways they design e-health initiatives and taking into account the resources which citizens do/not have for ICT Use for Health; and
- to apply the Framework to guide an analysis of data on the gendered use of ICTs for Health access from the EU survey (including use of ICTs for health purposes by women and mothers as health brokers for their families). We intend that this will then inform further qualitative investigation in this area across a range of countries, including Australia and Spain.
A potential challenge of working together could be combining quantitative and qualitative research from different paradigms, but "mixed methods" research is relatively common. We see that the framework will allow us to conduct quantitative work to provide data on 'big picture' patterns of ICT and e-health use across a population, and at the same time data on socioeconomic and demographic differences between and within different groups to highlight 'digital gradients'. It will collect and analyse data on a range of variables shown in Table 1. The qualitative research can then be linked to the quantitative work by recruiting citizens from groups of interest identified in the survey into focus groups or interviews. These would ask their perceptions of the reasons for why ICT use and e-health access differ according to the different categories shown in Table 1, as well as additional perspectives they have on ICT barriers and facilitators to their e-health use. In one of our earlier studies on what factors shape family size, the analysis of in-depth qualitative data provided new lines of inquiry which were then investigated through analysis of national Census data. This showed that university educated women who should be expected to have small family sizes were going against the trend if they stated in the Census that they belonged to certain Christian denominations (published in Newman & Hugo 2008). In our current work together, we expect to find that combining methodological approaches will similarly identify further nuances in ICT Use for Health purposes.
CONCLUSION
In conclusion, through combining our methodological approaches we hope to gain both a comprehensive picture of patterns and differential distribution of the Social Determinants of ICT Use for Health, and hence the in-depth story of the digital divide in e-health. This knowledge can then be used to inform policymakers and practitioners in the fields of the Information Economy/Digital Strategy and in Public Health about where to direct resources if they wish the E-Health Divide to be reduced. Our overall aim is to develop a program of research that will produce new knowledge to support policymakers and practitioners across a number of fields and disciplines to proactively shape ICT infrastructure and use across populations in ways that overcome the digital divide's potentially negative influence on equity in access to healthcare. We see this as increasingly important as health services and organisations move to greater online communication with citizens, who are not all ready or able to respond to the same degree.