Research Article
The Information Needs of Canadian Midwives and Their
Evidence Informed Practices: A Canada-Wide Survey
Lindsay Barnes
Research Support Officer
Faculty of Medicine and
Health
The University of Sydney
Sydney, New South Wales,
Australia
Email: [email protected]
Luanne Freund
Associate Professor
School of Information
University of British
Columbia
Vancouver, British Columbia,
Canada
Email: [email protected]
Dean Giustini
University of British
Columbia Biomedical Branch Librarian
VGH Diamond Health Care
Centre
Vancouver, British Columbia,
Canada
Email: [email protected]
Received: 4 Aug. 2019 Accepted: 29 Jan. 2020
![]() 2020 Barnes, Freund, and Giustini. This
is an Open Access article distributed under the terms of the Creative Commons‐Attribution‐Noncommercial‐Share Alike License 4.0
International (http://creativecommons.org/licenses/by-nc-sa/4.0/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
2020 Barnes, Freund, and Giustini. This
is an Open Access article distributed under the terms of the Creative Commons‐Attribution‐Noncommercial‐Share Alike License 4.0
International (http://creativecommons.org/licenses/by-nc-sa/4.0/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
DOI: 10.18438/eblip29616
Abstract
Objective – The study aim
was to
understand the extent to which Canadian registered midwives have access to and
make use of clinically relevant information for evidence
based midwifery practice.
Methods – A survey instrument was
created consisting of 17 multiple choice, matrix table, and
short answer questions and distributed to 1,690 recipients on the Canadian
Association of Midwives email list in fall 2018. In total, 193 responses were
included in the analysis.
Results – One third of midwives
do not have library
memberships. Midwives reported that limited access to clinically relevant
information is a key challenge in applying information in practice. Midwives
with library memberships reported more frequent use of high-quality information
while midwives without memberships reported more frequent use of websites.
Midwives with advanced degrees (graduate, PhDs) were more likely to be
high-frequency information users and rank themselves higher on evidence based competency scales than their
undergraduate-holding colleagues. Clinical practice guidelines were important
information sources and used frequently by midwives.
Conclusion – Midwives
reported low levels of academic or hospital library
memberships and yet used information frequently.
Clinical practice guidelines support the work of midwives but are
inaccessible to some due to paywalls. Midwives lacked confidence in evidence based practice and reported critical appraisal as
an area for development. Solutions to these problems could be addressed at the
hospital, health authority, provincial, or national association level, or
within midwifery departments at Canadian universities. Hospital and academic
libraries should prioritize the information needs of students and practicing
midwives and identify ways to foster use of library resources through
administrative or educational interventions.
Introduction
Midwives in Canada are autonomous care providers who
provide evidence based care for their clients
throughout pregnancy, birth, postpartum, and the newborn period. Midwives hold
a high degree of professional responsibility and accountability and must abide
by guidelines and standards appropriate to the clinical context (Ontario
Medical Association & Association of Ontario Midwives, 2005). According to
the Canadian Association of Midwives (CAM) (2015), “Midwifery practice is
informed by research, evidence-based guidelines, clinical experience, and the
unique values and needs of those in their care” (p. 2). This approach aligns with
evidence based medicine (EBM), defined by Guyatt, Rennie, Meade, and Cook (2008) as an approach to
patient care that uses best evidence to guide decision making and emphasizes
the importance of patient values and preferences.
Canadian midwives routinely integrate discussions about risk from the
literature into their conversations with clients (Van Wagner, 2016); further,
midwives must maintain their knowledge and clinical skills to ensure clients
are treated according to current best evidence (College of Midwives of Ontario,
2018). Research on the information behaviour and
evidence based practice (EBP) of Canadian midwives is lacking; however, a
growing number of international studies of midwives and nursing professionals
point to a gap between high level commitments to EBP and the actual practice of
it (Spenceley, O’Leary, Chizawsky,
Ross, & Estabrooks, 2008; De Leo, Bayes, Geraghty
& Butt, 2019). This is a serious issue, as noted by De Leo et al. (2019):
“The evidence‐to‐practice gap in maternity services remains a global issue for
midwives and demands prompt action from both knowledge producers and knowledge
users” (p. 4,234).
A recurring theme in this literature is the importance
of ease-of-information-access on practice. Canadian midwives are expected to
practice evidence based midwifery; however, the extent
to which midwives use and access sources of evidence—such as those found
through systematic reviews, original articles, or databases—is unknown. As
autonomous care providers, midwives have a great need to stay up to date;
however, midwifery associations do not operate libraries for their members.
This contrasts with other professional groups, such as the Canadian Nurses
Association and the College of Family Physicians of Canada, which have created
digital or physical libraries to provide members with access to current,
clinically relevant literature. While many summaries of the literature are
freely available online, key guidelines, policy statements, and committee
opinions from the Society of Obstetricians and Gynecologists of Canada (SOGC)
are published in the Journal of
Obstetrics and Gynecology of Canada which is accessible only to members of
the SOGC by subscription.
To understand the extent to which midwives are able to
satisfy their need for clinically relevant information, we conducted a survey
focused on the types of information sources midwives prefer and their
proficiency with and views about evidence based
practice given the dominant medical model of childbirth in Canada. The aim was
to examine cross-Canada access to and use of evidence based
information by midwives.
Literature Review
Midwifery Practice in Canada
The professionalization and regulation of midwifery in Canada developed
out of the women’s movement of the 1970s to offer an alternative to the
medicalization of pregnancy and childbirth (Parry, 2008). The Canadian
midwifery model of care is based on principles of professional autonomy,
continuity of care, informed choice, choice of birth place, collaborative care,
and evidence based practice (Canadian Association of Midwives,
2015). In this model, a midwife is a responsible and autonomous community-based
provider working in partnership with women and their families to balance
patient values with community standards of practice and current best evidence
(College of Midwives of Ontario, 2018).
Midwifery Education Programs (MEPs) in Canada are direct-entry,
four-year undergraduate degrees leading to a Bachelor of Midwifery or Bachelor
of Health Sciences. There are “bridging” or “pre-registration” midwifery
programs for internationally educated midwives who seek to practice in Canada
(College of Midwives of British Columbia, n.d.). During their time as students,
midwives have access to library databases and electronic resources through
their universities. Upon completion of their programs of study, their access to
university library collections ends or is restricted to alumni privileges or
library walk-in access.
Funding models for midwifery practice vary by province and territory,
but most midwives work as independent contractors under a fee-for-service
agreement with their home province (British Columbia, Alberta, and Ontario) or
under a salaried model (Manitoba, Saskatchewan, the Northwest
Territories and Quebec). While no studies have been conducted on
the advantages of each model with respect to library access or use of
clinically relevant information, under the fee-for-service model “midwives have
greater flexibility and fewer bureaucratic barriers to establishing midwifery
practice in diverse geographic settings” (Thiessen, Haworth-Brockman, Nurmi, Demczuk, & Sibley, 2018, p. 7). Fee-for-service
encourages the establishment of midwifery practices at a distance from
hospitals and their onsite libraries and professional networks. In comparison
to other jurisdictions, such as the U.K. and Australia, midwives practicing in
Canada experience a greater degree of autonomy and a greater responsibility to
proactively consult and collaborate with other health professionals (Mallot et al., 2009).
Information Seeking and Evidence Based Practice
Two studies offer useful conceptual frameworks for this project. Leckie,
Pettigrew, and Sylvain (1996) proposed a model of the information seeking of
professionals, taking into account their roles, tasks,
and information needs. As primary care providers, midwives’ roles overlap with
both physicians and nurses, indicating a broad range of information needs. The
model identifies certain constants across professional groups, including the
importance of information access, and it points to a high degree of complexity
in professional work settings, which leads to variability and unpredictability
in information seeking (Leckie et al., 1996). The second model (Spenceley et al., 2008) identifies a range of factors that
shape information seeking activity and outcomes in evidence based nursing
practice: the context of practice, which includes aspects of the individual
practitioner (e.g., education, skills, attitudes), the work setting (e.g.,
training, information resources); the sources of information, which have
attributes, such as availability and trustworthiness; and a number of mediating
factors such as time pressures, the expectations of others, and situational
barriers. Notable themes include the constraints of time and access to
information on the search process, the need for administrative support for EBP,
and the preference for trusted interpersonal sources of information (Spenceley et al., 2008). Both frameworks situate
information practices in context and highlight the awareness of and access to a
range of sources for diverse tasks in complex work settings.
Although studies of information seeking and EBP of Canadian midwives are
lacking, studies of midwives and nurses from the U.K. and Australia indicate
that EBP is consistent with the philosophy of midwifery and is valued by
practitioners (Bayes, Juggins, Whitehead & De Leo, 2019; De Leo et al.,
2019; Fairbrother, Cashin, Conway, Symes, & Graham, 2016; Toohill, Sidebothan, Gamble,
Fenwick, & Creedy, 2017; Veeremah, 2016).
Notably, EBP has been recognized by midwives as a means to reduce the
medicalization of pregnancy and birth, including the overuse of interventions
(De Leo et al., 2019; Kennedy, Doig, Hackley, Leslie & Tillman, 2012;
Miller et al., 2016). At the same time, there is considerable evidence that
midwifery care is not always reflective of EBP guidelines, raising questions as
to the reasons for this gap (Bayes et al., 2019; De Leo et al., 2019;
Fairbrother et al., 2016; Toohill et al., 2017).
A recent integrative review of midwives’ EBP sought to investigate this
issue through close examination of six studies, several of which included both
nurses and midwives (De Leo et al., 2019). The authors identified a number of
themes. Practitioners are aware of EBP and confident with their skills;
however, published information sources are underused, with practices based more
on convention and information gained from patients and other professionals
(Bayes et al., 2019; Fairbrother et al., 2016; Heydari
et al., 2014). For example, in a survey of 297 Australian midwives to evaluate
the uptake of evidence based guidelines on normal
birth, Toohill et al. (2017) found that almost all
respondents were familiar with the guidelines, but only 71% routinely used
them. Three barriers to EBP implementation are widely identified: a lack of
time to find and use evidence based resources (Bayes et al., 2019; Fairbrother
et al., 2016; Toohill et al., 2017; Veeramah, 2016); organizational barriers, such as
resistance to change, lack of support from colleagues, and structural
impediments (Bayes et al., 2019; Heydari et al.,
2014; Toohill et al., 2017; Veeramah,
2016); and limited access to information and computers in the workplace
(Fairbrother et al., 2016; Toohill et al.; 2017; Veeramah, 2016).
Information Literacy and Skills Training
Training medical practitioners to search and appraise high-quality
evidence has long been recognized as an important factor in the provision of
patient care (Guyatt, Meade, Jaeschke,
Cook, & Haynes, 2000). Informed clinicians are able to assess their own
knowledge gaps and formulate effective research questions (McKibbon,
Wyer, Jaeschke, & Hunt,
2008). Lack of access to libraries has been identified as an obstacle to
developing these skills among physicians (Coumou
& Meijman, 2006). In an early survey of the
information needs of 1,715 U.K. nursing professionals, including midwives, Bertulis and Cheeseborough (2008)
found that lack of training in information seeking was an obstacle to applying
evidence in practice. More recent research continues to identify education and
training gaps (e.g. Veeramah, 2016) and the need for
capacity building among nurses and midwives (Fairbrother et al., 2016),
although there is evidence that EBP skills are rising over time. A survey of
Australian nurses and midwives found higher self-reported expertise compared to
earlier studies conducted in the U.K. and Australia (Fairbrother et al., 2016).
However, less than 40% of respondents considered themselves competent or expert
at finding research evidence or using the library to locate information. Rates
of Internet competency were higher, at 63%, a finding supported by additional
research on Australian midwives (McKenna & McLelland,
2011).
Longstanding information practices, including source
preferences, also impact EBP. Ebenezer (2015) reviewed the literature on the
information behaviour of nurses and midwives between
1998 and 2014 and identified a strong preference for gaining information
through human sources. This preference for what Estabrooks
et al. (2005) terms “interactive” and “experiential” sources of information
over formal or “documentary” sources (p. 471) is one of the most frequent
findings in studies of information seeking of nursing and midwives (Bertulis & Cheeseborough,
2008; De Leo et al., 2019; Ebenezer, 2015; Fairbrother et al., 2016; Ricks
& Ham, 2015; Thompson et al., 2001b). Interestingly, this preference for
social information sources does not seem to extend to social media. Dalton et
al. (2014) conducted a mixed methods study of information communication
technology use among Australian midwives and found a high degree of consensus
that social media is an inappropriate and high-risk means of sharing
information in a healthcare context.
Use of pre-appraised evidence, such as practice guidelines,
systematic reviews, and computer decision support systems, continues to impact
the quality of clinical decision making. Guyatt,
Mead, Jaeschke, Cook, and Haynes (2000) noted the
critical importance of pre-appraised evidence for clinicians and observed that,
while not technically practicing evidence based care, the clinical trainees
whom they studied acquired a “restricted set of skills” which included the
ability to track down and use secondary sources of pre-appraised evidence (p.
955). Lafuente-Lafuente et al. (2019) found that
health practitioners used primary evidence infrequently which “suggests that
many professionals probably do not (or are unable to) verify independently, by
their own means, the validity of what is stated in guidelines, or otherwise
what is presented to them as ‘EBM-based’” (2019, p. 5). This is supported by
the work of Fairbrother et al. (2016), which found that articles published in
research, nursing, and medical journals were the least frequently used sources
of information in practice.
Summary
The gap between EBP commitments and reliance upon evidence in every day
practice is widely documented among midwives and the nursing professionals more
generally. This situation persists across the diverse national contexts and workplace
settings in which midwives practice. Relevant models
of information seeking stress the complex and situated nature of the work of
health professionals, in which the roles, tasks, information sources, and work
environments significantly shape and constrain practices. A broad, but
generally consistent, set of barriers to EBP in midwifery have been identified
in studies conducted outside Canada. Among these, access to resources, EBP
literacies and skills, and longstanding information practices are key. Other
factors also emerge as important, notably time, organizational culture, and
receptivity to change. Canadian midwives operate with more autonomy than their
colleagues in the U.K. and Australia, where the majority of studies have been
conducted, which suggests that these findings may not generalize to the
Canadian context.
Aims
Rather than examining the full range of factors known
to shape EBP, the current study focuses on access to libraries and information,
source use, and EBP literacies in the Canadian context, as a first step towards
understanding the local situation and constraints upon EBP. A survey was
designed to investigate the extent to which Canadian registered midwives had
access to and made use of clinically relevant information in practice. The research questions were: How frequently do Canadian midwives use
published information and which sources do they prefer? What challenges do they
encounter in accessing and using information? How do they acquire the
information literacy skills needed to find and apply clinical information and
are those skills well-developed? To provide a more nuanced picture of the status quo, we compare responses across
several factors, including region, work conditions and settings, and access to
libraries.
Methods
Survey Design
The survey instrument (see Appendix) was developed
iteratively by soliciting feedback from library and midwife professionals. The
range and types of questions were developed by using the Association of College
& Research Libraries’ “Information
Literacy Competency Standards for Nursing” (Association of
College and Research Libraries, 2013).
The frameworks of Leckie et al. (1996) and Spenceley
et al. (2008) indicated the importance of collecting contextual data on
demographics, specialization, career stage, and other factors likely to
influence information behaviour. An early version of
the questionnaire was piloted with two registered midwives, both educators, and
a health librarian from British Columbia, Canada. The final version incorporated
feedback from the pilot sessions.
The questionnaire begins by asking for demographic
data to establish the personal and practice context (Q1-6). The next set of
questions (Q7-10) focuses on general access and use of information, including
library memberships and frequency of use of information. Q11 asks about
information source types and use frequency. The list of information sources was
derived from the work of McKibbon et al. (2008).
These categories were not explicitly defined in the questionnaire, but were
presented with illustrative examples, as follows:
·
Summaries (clinical practice guidelines and systematic
reviews)
·
Textbook-like e-resources (UpToDate, AccessMedicine)
·
Studies (original research articles)
·
Print books (monographs, textbooks)
·
Apps
·
Popular websites (WebMD, Mayo Clinic)
·
Social media (Twitter)
Q12 asks participants to rate challenges in applying
clinically relevant information, with a focus on access and literacy skills.
The final set of questions (Q14-16) ask about information literacy training and
competencies. Q14 asks participants to report on their level of expertise in
EBP using a five-point scale ranging from novice to expert, across four
categories of EBP competencies (Q14). Using this data, we calculated an
aggregate metric of EBP competency using the sum of the responses across the
four areas converted to a score out of 10 for ease of interpretation, such that
an expert level of competency across all areas received a top score of 10. This
metric allowed us to compare self-reported EBP competency levels across groups.
The study received approval from the Behavioural Research Ethics Board at the University of
British Columbia. The questionnaire was implemented and distributed online
using the Qualtrics platform.
Study Responses and Recruiting
Survey responses were collected during the fall of
2018. The study population was registered midwives in Canada, of which there
were 1,690 at the time of the study (Canadian Association of Midwives, 2018).
CAM is the national body representing midwives and it collects and maintains a
database of registered midwives using data from provincial and territorial
associations and colleges. All registered midwives in the database (n = 1,690) received an invitation from
CAM to participate. To encourage further participation, we distributed
invitations through the Midwives Association of British Columbia’s email list
and the Canadian Registered Midwives Facebook group, which served as reminders
or reinforcements. No compensation was provided for completing the
questionnaire, which took, on average, five to 10 minutes. In total, 218
midwives participated in the survey, representing a 12.8% response rate. Of the
218 questionnaires submitted, 25 were found to be substantially incomplete and
were removed, leaving 193 questionnaires for analysis.
Responses were received from eight provinces and one
territory, but most respondents were from Ontario (40%) and British Columbia
(BC, 39%), followed by Alberta (8%) and Quebec (6%). The mean number of years
of respondents’ midwifery practice was nine, with responses ranging from zero
to 40 years. The educational profile of respondents included 67% (n = 130) holding a Bachelor degree, 23%
(n = 44) Master’s degree, and 4% (n = 7) PhD. A small number held other
credentials. A majority of respondents (71%, n = 137) were practicing full time with 17% (n = 32), practicing part time, 7% (n = 13) non-practicing, many of whom were educators, and 6% (n = 11) reporting some other status,
including those on temporary leaves. We reviewed the responses from the last
two categories and determined that these responses were valid for our purposes,
as these were experienced midwives, whose responses were consistent with the
broader sample.
Table 1 summarizes the distribution of responses by
province and work setting. The majority (68%, n = 131) of respondents were practicing in an urban or suburban
setting, while 26% (n = 51) were
rural and 6% (n = 11) remote. These
categories were provided to participants without definitions, and so were
subject to interpretation. Given the low number of responses from most
provinces, we report comparisons by province only for BC and Ontario in this
report. The BC-Ontario comparisons are not meant to be representative of
conditions across Canada and are not generalizable. Rather, the data analysis
is descriptive in nature and is meant to provide a starting point for
examination and further research.
Table
1
Distribution
of Responses by Region and Work Setting
|
Urban |
Suburban |
Rural |
Remote |
Total |
|
|
Alberta |
11 |
3 |
2 |
16 (8%) |
|
|
British Columbia |
36 |
10 |
24 |
3 |
73 (38%) |
|
Manitoba |
3 |
3 (2%) |
|||
|
New Brunswick |
1 |
1 (1%) |
|||
|
NW Territories |
1 |
1 (1%) |
|||
|
Nova Scotia |
1 |
2 |
3 (2%) |
||
|
Ontario |
36 |
19 |
20 |
3 |
78 (40%) |
|
Quebec |
4 |
3 |
2 |
3 |
12 (6%) |
|
Saskatchewan |
1 |
1 (1%) |
|||
|
Multiple provinces |
2 |
1 |
3 (2%) |
||
|
Other |
|
1 |
|
1 |
2 (1%) |
|
Grand total |
95 (49%) |
36 (19%) |
51 (26%) |
11 (6%) |
193 |
Results
Library Membership
We asked participants if they held membership in an
academic or hospital library, based on the assumption that library privileges,
such as access to bibliographic databases and electronic resources, require
library membership. Figure 1 summarizes responses. Overall, 67% (n = 129) of respondents reported some
type of academic library membership and 33% (n = 64) reported having no library membership (or unsure). Of those
who had membership, 53% (n = 68) had
access through a university as a student, employee, or faculty member; 57% (n = 74) through a hospital; and 9% (n = 12) through a college or private
library. Many had access through multiple avenues. Several respondents
indicated in their comments that they held alumni library privileges, which
were described as “limited” or due to expire one year after graduation. Others
said they gained access to academic collections through use of their
colleagues’ or partners’ passwords or via credentials gained through other
professional associations. One respondent added the comment that “hospitals
refuse midwives access.”

Figure 1
Library membership (academic or hospital
libraries).
We compared the rates of library membership across
different geographic regions. A higher percentage of respondents from BC (74%)
reported having membership access compared to those from Ontario (65%). With
respect to work setting (Figure 2), rates of library membership in urban work
environments were highest at 72% followed by suburban at 69%, remote at 64%,
and rural at 57%. Midwives with graduate degrees reported higher levels of
library membership (78%) compared to those with undergraduate degrees (62%).
There was no difference between those who reported working full time or part
time. In a separate question, we asked if respondents used public libraries as
a resource for their clinical information needs. This proved to be highly
uncommon, with 96% of respondents indicating that they very rarely or never use
public libraries to stay informed for practice.

Figure 2
Library membership by
work setting (percent).
Use of Clinically Relevant Information
Participants were asked how frequently they refer to clinically relevant
information in their midwifery practices. The most common response was:
frequently – several times a week (65%), followed by occasionally – a few times
a month (18%), and very frequently – several times a day (14%). Figure 3
compares the frequency of information usage by those with and without
membership in an academic or hospital library. Not surprisingly, a higher
percentage of those with access to a library reported using information at a
high frequency, while those without access were more likely to use information
occasionally, rarely, or very rarely.

Figure 3
Comparison of information use frequency by
library membership.
Group comparisons were made based on high-frequency information usage
(defined as the percentage of those who reported using information frequently
or very frequently):
·
85% (n = 62)
of respondents from BC were high-frequency users compared to 76% (n = 59) in Ontario;
·
85% (n = 81)
of respondents in urban settings were high-frequency users compared with 72% (n = 26) in suburban, 73% (n = 37) in rural, and 82% (n = 9) in remote settings;
·
82% (n = 113)
of respondents working full time were high-frequency users compared with 63% (n = 40) of those working part time;
·
88% (n = 45) of respondents with graduate
degrees were high-frequency users compared with 77% (n = 96) of those with undergraduate degrees.
Participants were asked to report on their use of nine different types
of information sources in terms of frequency. The results, presented in Figure
4 showing higher percentages in darker shading, indicate summaries and
colleagues are used most frequently as information sources.

Figure 4
Heat map of information source frequency of use (percent).
We were interested in the impact of library access on
the types of information sources consulted. We focused our analysis on a subset
of all information source types, including those we thought would be most
affected. The results, presented in Table 2, showed some interesting patterns.
At the highest level of frequency, those without library access reported less
frequent use of summaries, colleagues, and textbook-like e-resources and more
use of websites than colleagues with library access. Research articles were
used less frequently by those without access, although this shows up in the frequent
(lower) and rare (higher) use categories. Lack of membership did seem to
influence resource use patterns, but it did not prevent most midwives from
using a range of resource types on a regular basis.
Table 2
Comparison of Information Source Frequency of
Use (Percent) by Library Membership (Yes/No)
|
Very Frequently |
Frequently |
Occasionally |
Rarely |
Never |
||||||
|
Information Sources |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
No |
|
Summaries |
48 |
40 |
44 |
48 |
8 |
12 |
0 |
0 |
0 |
0 |
|
Colleagues |
40 |
31 |
51 |
48 |
8 |
17 |
2 |
3 |
0 |
0 |
|
Textbook-like e-resources |
21 |
10 |
37 |
28 |
28 |
33 |
10 |
17 |
5 |
12 |
|
Original research articles |
10 |
10 |
36 |
20 |
43 |
45 |
11 |
22 |
1 |
3 |
|
Popular websites |
5 |
15 |
33 |
27 |
41 |
42 |
17 |
10 |
5 |
7 |
Borrowed Library Access
In the final open-ended question in the survey, a number of responses
raised concerns that midwives are forced to ask for help in accessing essential
information. One midwife commented “I always meet my information needs by using
online resources or by asking my senior student to use her online connection to
university libraries to locate resources…” Another stated, “I don't have other
means of ‘official’ access but I frequently use a family member’s library card
to access the University library.” Other respondents mentioned using a
partner’s university library membership and a friend’s login to UpToDate. Many
midwives noted that they had alumni library privileges but commented on the
limitations of such access, especially in cases where such privileges do not
extend to online databases.
Library Skills and Evidence Based Practice Competencies
Question 14 asked participants with multiple choice
and an optional short answer question if they had ever received library skills
training. Twenty-eight percent reported that they had never received training
(or could not remember). Overall, 54% reported receiving some library skills
training during their midwifery education and training, and the remaining 18%
had exposure to this training through other means. Those who made additional comments
for this question noted that such training was “limited,” or superficial: “we
touched on it.” Several respondents noted that they received more training in
library skills during the acquisition of degrees unrelated to midwifery. Other
comments highlighted that training was brief, years ago, and that the specifics
of the instruction were difficult to recall:
·
“This training was 10-15 years ago. A lot has changed
since then.”
·
“But I can’t call on that knowledge even though it’s
been 7-10 years.”
·
“20 years ago, too long ago”
Participants reported interest in receiving library
skills training; however, a number of comments indicated that training would
not be useful without access to library resources.
Results of the EBP competency question summarized in
Figure 5 indicate that very few respondents identified as expert in any of the
EBP competency areas, and the majority of responses were in the middle points
of the scale. The highest levels of expertise were reported for converting the
need into an answerable question and application of evidence to practice and
the lowest levels for critical appraisal of evidence.
Using an aggregate metric of EBP competency, we
compared competency scores across groups. Self-reported competency scores
increase with experience, with mean scores of 5.7 for those with less than 5
years in practice; 6.0 for those with between 5 and 19 years, and 6.5 for those
with 20 or more years. Similarly, higher competency levels are reported for
those with graduate level education (6.4 for Master’s and 7.1 for PhD) as
compared to those with undergraduate degrees (5.7). Respondents with library
access report higher levels of expertise (6.0) than those who do not report
access to a library (5.5).
Challenges to Using Clinically Relevant Research in Practice
Participants were asked to indicate their level of
agreement with a set of five challenges as factors in their own practice.
Figure 5 summarizes the results, showing the percent of all respondents who
indicated agreement or strong agreement with each statement. Lack of access to
information showed the highest level of agreement (53%), followed by the
difficulty in judging the quality of research (41%), which reinforces the low
self-reported competency in this area.
Further analysis regarding the challenges associated
with lack of information access suggests that some variation exists across
groups:
·
62% (n = 31)
of midwives working in rural settings agreed that information access was a
challenge in comparison with 47% (n = 45)
of those working in urban settings;
·
66% (n = 51%)
of early career midwives agreed that information access was a challenge in
comparison with 29% (n = 6) of those
with more than 20 years’ experience;
The high costs of paying to download articles and buy
memberships to point of care tools such as UpToDate were mentioned repeatedly
in response to the open question. Comments included the following:
- “I think the biggest limitation is access to
information. SOGC guidelines, UpToDate and several other critical sources
are now fee for service and some midwifery clinics will not pay these fees,
leaving the midwives at a disadvantage for relevant data.”
- “Subscriptions to library databases is very
expensive particularly for small practices or individual midwives.”
- “The main barrier to accessing medical libraries
and online journals is cost. For a midwifery clinic or individual midwife
to afford this they need to pay midwives adequately.”
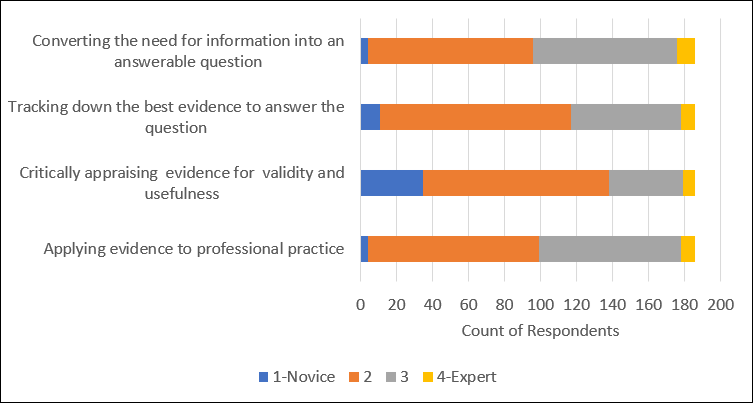
Figure 5
Levels of reported
expertise across EBP competency areas.

Figure 6
Levels of agreement with
challenges to using clinically relevant research in midwifery practice.
Discussion
This study set out to understand the extent to which Canadian midwives
have access to and make use of clinically relevant information in practice. One
third of survey respondents reported having no library membership. Urban
midwives and those with graduate degrees reported higher levels of library
membership. This level of access is consistent with Veeremah’s
(2016) study, in which one third of respondents reported limited access to
information, and it affirms prior research indicating that access to
information continues to be a challenge in professional contexts (Leckie et
al., 1996; Spenceley et al., 2008), even as digital
and mobile information technologies proliferate. Results further show that
those respondents without library access were less likely to be frequent users
of clinically relevant information and were more likely to refer to websites,
which undergo less quality control than published summaries, textbook-like
e-resources, or research articles. Considering the high degree of
responsibility and technical knowledge required in midwifery, this finding is
concerning, as it brings into question the quality, consistency, and equity of
care across settings. While other health practitioners in Canada enjoy access
to digital libraries offered by their colleges and associations, midwives do
not benefit from such a program, which could be considered a basic component of
EBP.
More than 50% of survey respondents agreed that access to information is
an obstacle to EBP, with more limited agreement that finding, using, and
evaluating clinically relevant information is challenging. A surprising result
was that respondents reported finding creative ways to access the information
they needed for EBP by bypassing paywalls and borrowing memberships. One
respondent linked this issue of information access with the broader issue of
hospital integration and hospital privileging, by indicating that they were denied
access to information by the hospital. If midwives are barred from using
library services by virtue of not being “staff” and holding “privileges,” this
bureaucratic barrier raises ethical implications for patient safety and should
be addressed as a matter of urgency. In this context, “borrowing” access
privileges, which breaks licensing agreements and constitutes a misuse of
library systems, can be viewed as a form of activism designed to redress an
imbalance of power and privilege within the healthcare field. While this study
did not examine the impact of organizational factors on EBP, studies such as
that carried out by Bayes et al. (2016) show that midwives are vulnerable to
opposition to EBP from hospitals, colleagues, and superiors, in part because
EBP guidelines may run counter to dominant medicalized approaches to childbirth
(Toohill et al., 2017). This perspective should be
explored further, as the role of power and privilege in information seeking and
EBP is largely absent from prior research and existing conceptual frameworks
(e.g. Leckie et al., 1996; Spenceley et al., 2008),
and it may offer new insights, particularly for the study of midwifery in
Canada.
The majority of midwives reported difficulty judging
the quality of the evidence. This finding is echoed in studies by Fairbrother
et al. (2016) and by Ross (2010) who reported that nurses had difficulty
understanding articles and had insufficient skills critiquing the literature.
Midwives indicated that the information literacy skills they received during
their education was limited and, in many cases, stale. However, midwives with
advanced degrees (graduate, PhDs) ranked themselves more highly on evidence based practice competency scales than their
undergraduate-holding colleagues. Guyatt et al.
(2000) considered the skills of critical appraisal of primary studies to be
invaluable, stating that health care providers who had these skills would be
better able to identify when attempts to influence practice were made based on
evidence (or to justify childbirth interventions). Lafuente-Lafuente
et al. (2019) echo this sentiment, stating that practitioners who used primary
studies infrequently were less able to independently verify the guidance
provided in clinical practice guidelines. In the context of increasing
childbirth interventions, midwives with quality appraisal skills of original
literature may be better able to identify when clinical guidelines are out of
date, biased, or have used poor methodology. This finding points to the fact
that increasing the accessibility of information is only one component of a
much broader set of challenges, which includes the need for training and
capacity building.
Results of this study reinforce previous findings that clinical practice
guidelines are an essential resource for clinicians. In total, 91% of midwives
in this study reported frequent use of summaries such as those published by the
Society of Obstetricians and Gynecologists of Canada, the Association of
Ontario Midwives (AOM), and the Perinatal Services of British Columbia.
However, clinical practice guidelines developed by the SOGC are currently
behind a membership firewall, despite their relevance for maternity care
professionals. Membership in SOGC is fee-based ($160 per year) and many midwives
in this study indicated that they did not have access to these guidelines. The
College of Midwives of British Columbia recently rescinded their clinical
practice guidelines (which were freely available on their website), and no
longer create or maintain them due to a lack of funding and the existence of
guidelines from national expert bodies such as the SOGC and the Perinatal
Services of British Columbia (R. Comfort, personal communication, July, 10,
2019). This decision is concerning in light of the findings of this study and
because midwife-specific guidelines address the person-centered model of care
that characterizes Canadian midwifery.
The opinions of trusted colleagues were the second most common
information source used by surveyed midwives, which is not surprising given
that this is one of the most consistent themes in the information-seeking
research on professionals, nurses, and midwives (De Leo et al., 2019; Leckie et
al., 1996; Spenceley et al., 2008). While this
research did not examine why this is the case, it is clear from the wider
literature that interpersonal sources of information are valuable in the
context of EBP for a number of reasons, including that people provide
information that is contextualized and experience based, and in some cases they
perform a translational role, by sharing information in a form that is more
easily understood or made more relevant for a particular audience (Thompson et
al., 2001b). Given this preference for collegial information sharing,
mentorship or peer-based training models for EBP in midwifery may prove to be
effective (Fairbrother et al., 2016). At the same time, the reliance on
colleagues as information sources reinforces the role that a supportive
organization plays in enabling EBP, including midwife leaders able to champion
change (Bayes et al., 2019; Spenceley, et al., 2008).
This study has focused only on select components of the conceptual
frameworks developed by Leckie et al. (1996) and by Spenceley
et al. (2008), notably, aspects of the individual (education, work experience,
skills); the work setting (region, employment status); the sources of
information (accessibility, source type); and the outcomes (information behaviours). Results are based on limited self-report data
and statistical tests were not conducted. Therefore, these results are not
generalizable. A more comprehensive study would need to consider additional
features, notably, the impact of organizational factors and time pressures,
which are known to influence EBP. Given the lack of prior research in the
Canadian context and the unique nature of midwifery practice in Canada, further
research is needed to validate and extend these findings. One contribution of
this study is the identification of information-seeking strategies that sidestep
existing systems and norms in order to meet needs, and which may reflect
structural barriers and power imbalances that are not currently addressed in
these models.
Conclusion
Canadian midwives, as experts in physiologic birth, enjoy an expanded scope
of practice that requires frequent and ongoing consultation with information.
As professionals committed to EBP, access to high-quality information would
seem to be a given; however, the results of this survey indicate that a substantial number of midwives are practicing
without such access. Clinical practice guidelines support the work of midwives
but are inaccessible to many midwives due to paywalls. Respondents lacked
confidence in evidence
based practice and
reported critical appraisal as an area for development. While no Canadian
universities currently offer higher degrees in midwifery, it may be that future
offerings of advanced midwifery programs would have a beneficial effect on evidence based practice proficiency as midwives with
advanced degrees had higher self-reported EBP expertise. Coordinating access to
digital biomedical collections or removing barriers to midwife access of these
collections is one way that hospitals, health authorities, and their libraries,
provincial, or national associations could help midwives
practice EBP. Hospital and academic libraries should prioritize the information
needs of student and practicing midwives and identify ways to foster use of
library resources through educational interventions.
Acknowledgements
We would like to thank all those midwives who responded to the
questionnaire and shared their experience and insights. We appreciate the
support of the CAM for allowing us to recruit via their listserv, and to Cathy
Ellis, RM, Alixandra Bacon, RM, and Brooke Ballantyne
Scott, Manager of Library Services, Royal Columbian Hospital, who provided
comments and a review of the survey instrument.
References
Association of College and Research Libraries. (2013).
Information literacy competency standards for nursing. Retrieved from http://www.ala.org/acrl/standards/nursing
Bayes, S., Juggins, E., Whitehead, L., & De Leo, A. (2019).
Australian midwives’ experiences of implementing practice change. Midwifery, 70, 38–45. https://doi.org/10.1016/j.midw.2018.12.012
Bertulis, R., & Cheeseborough, J. (2008). The
Royal College of Nursing’s information needs survey of nurses and health
professionals. Health Information and
Libraries Journal, 25(3),
186–197. https://doi.org/10.1111/j.1471-1842.2007.00755.x
Canadian Association of Midwives. (2015). Canadian
midwifery model of care [position statement]. Retrieved from https://canadianmidwives.org/wp-content/uploads/2018/10/FINALMoCPS_O09102018.pdf
Canadian Association of Midwives. (2018). Midwifery care
for all: Building the profession, annual report, 2017-2018. Retrieved from https://canadianmidwives.org/wp-content/uploads/2018/10/Annual-Report-2017-2018.pdf
College of Midwives of British Columbia (n.d.).
Recognized midwifery education programs. Retrieved from https://www.cmbc.bc.ca/registration/inter-provincial-registration/recognized-midwifery-education-programs/
College of Midwives of Ontario. (2018). Professional
standards for midwives. Retrieved from https://www.cmo.on.ca/wp-content/uploads/2018/06/Professional-Standards.pdf
Coumou, H. C., & Meijman, F. J. (2006). How do
primary care physicians seek answers to clinical questions? A literature review. Journal of the
Medical Library Association, 94(1),
55–60. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16404470
Dalton, J. A., Rodger, D. L., Wilmore, M., Skuse, A. J., Humphreys, S., Flabouris,
M. & Clifton, V.L. (2014). “Who’s afraid?”: Attitudes of midwives to the
use of information and communication technologies (ICTs) for delivery of
pregnancy-related health information. Women
and Birth, 27(3), 168-173. https://doi.org/10.1016/j.wombi.2014.06.010
De Leo, A., Bayes, S., Geraghty, S. & Butt, J.
(2019). Midwives’ use of best available evidence in practice: An integrative
review. Journal of Clinical Nursing, 28, 4225-4235. https://doi.org/10.1111/jocn.15027
Ebenezer, C. (2015). Nurses’ and midwives’ information
behaviour: A review of literature from 1998 to 2014. New Library World, 116(3/4), 155–172. https://doi.org/10.1108/NLW-07-2014-0085
Estabrooks. C. A, Rutakumwa, W., O’Leary, K. A., Profetto-Mcrath, J., Milner, M., Levers, M. J. &
Scott-Findlay, S. (2005). Sources of practice knowledge among nurses. Qualitative Health Research, 15(4), 460-476. https://doi.org/10.1177/1049732304273702
Fairbrother, G., Cashin, A., Conway, R., Symes, A.,
& Graham, I. (2016). Evidence based nursing and midwifery practice in a
regional Australian healthcare setting: Behaviours,
skills and barriers. Collegian, 23(1), 29–37. https://doi.org/10.1016/j.colegn.2014.09.011
Guyatt, G., Meade, M.,
Jaeschke, R., Cook, D., & Haynes, R. (2000).
Practitioners of evidence based care. Not all
clinicians need to appraise evidence from scratch but all need some skills. BMJ (Clinical Research Ed.), 320(7240),
954–955. https://doi:10.1136/bmj.320.7240.954
Guyatt, G., Rennie, D., Meade, M. & Cook, D. (2008). Users’ Guides to the Medical Literature: A Manual for Evidence-Based
Clinical Practice (2nd edition). New York, NY: McGraw-Hill.
Heydari, A., Mazlom, S., Ranjbar,
H., & Scurlock‐Evans, L. (2014). A study of Iranian nurses and midwives’
knowledge, attitudes, and implementation of evidence‐based practice: The time
for change has arrived. Worldviews on
Evidence Based Nursing, 11(5),
325–331. https://doi.org/10.1111/wvn.12052
Kennedy, H. P., Doig, E., Hackley, B., Leslie, M. S.,
& Tillman, S. (2012) “The midwifery two step”: A study on evidence-based
midwifery practice. Journal of Midwifery
& Women’s Health, 57(5), 454-460. https://doi.org/10.1111/j.1542-2011.2012.00174.x
Lafuente-Lafuente, C., Leitao, C., Kilani,
I., Kacher, Z., Engels, C., Canoui-Poitrine,
F., & Belmin, J. (2019). Knowledge and use of
evidence-based medicine in daily practice by health professionals: A
cross-sectional survey. BMJ Open, 9,
1-6. https://doi.org/10.1136/bmjopen-2018-025224
Leckie, G., Pettigrew, K., & Sylvain, C. (1996).
Modeling the information seeking of professionals: A general model derived from
research on engineers, health care professionals, and lawyers. The Library Quarterly, 66(2), 161-193.
Malott, A., Davis, B., McDonald, H., & Hutton, E. (2009). Midwifery
care in eight industrialized countries: How does Canadian midwifery compare? Journal of Obstetrics and Gynaecology Canada, 31(10),
974–979. https://doi.org/10.1016/S1701-2163(16)34328-6
McKenna, L. & McLelland, G. (2011)
Midwives’ use of the Internet: an Australian study. Midwifery, 27(1), 74-79. https://doi.org/10.1016/j.midw.2009.07.007
McKibbon, A., Wyer, P., Jaeschke, R., &
Hunt, D. (2008). Finding the evidence. In G. Guyatt,
D. Rennie, D. Cook, M. Mead & American Medical Association (Eds.), Users Guides to the Medical Literature
(pp. 29-58). New York, NY: McGraw Hill.
Miller, S., Abalos, E., Chamillard, M., Ciapponi, A., Colaci, D., Comandé, D., … Althabe, F. (2016). Beyond too
little, too late and too much, too soon: A pathway towards evidence-based,
respectful maternity care worldwide. Lancet,
388(10056), 2176-2192. https://doi.org/10.1016/S0140-6736(16)31472-6
Ontario Medical Association & Association of
Midwives of Ontario (2005). A joint statement of professional relations between
obstetricians and midwives in Ontario [position statement]. Retrieved from https://www.ontariomidwives.ca.
Parry, D.C. (2008). “We wanted a birth experience, not
a medical experience”: Exploring Canadian women’s use of midwifery. Health Care for Women International, 29(8-9), 784-806. https://doi.org/10.1080/07399330802269451
Ricks, E., & Ham, W. (2015). Health information
needs of professional nurses required at the point of care. Curationis, 38(1), 1-8. https://doi.org/10.4102/curationis.v38i1.1432
Ross, J. (2010). Information literacy for
evidence-based practice in perianesthesia nurses:
Readiness for evidence-based practice. Journal
of Perianesthesia Nursing, 25(2), 64-70. https://doi.org/10.1016/j.jopan.2010.01.007
Sackett, D., Strauss, S., Richardson, W., Rosenberg,
W., & Haynes, R. (2000). Evidence-based medicine: How to practice and teach EBM
(2nd ed.) Edinburgh: Churchill Livingstone.
Spenceley, S.M., O’Leary, K.A., Chizawsky, L.L.K.,
Ross, A.J., & Estabrooks, C.A. (2008). Sources of
information used by nurses to inform practice: An integrative review. International Journal of Nursing Studies,
45(6), 954-970. https://doi.org/10.1016/j.ijnurstu.2007.06.003
Thiessen, K., Haworth-Brockman, M., Nurmi, M., Demczuk, L., & Sibley, K. (2018). Delivering midwifery:
A scoping review of employment models in Canada. Journal of Obstetrics and Gynaecology Canada,
42(1), 61-71. https://doi.org/10.1016/j.jogc.2018.09.012
Thompson, C., McCaughan, D., Cullum, N., Sheldon, T., Mulhall, A., &
Thompson, R. (2001). Research information in nurses
clinical decision making: What is useful? Journal
of Advanced Nursing, 36(3),
376-388.
https://doi.org/10.1046/j.1365-2648.2001.01985.x
Toohill, J., Sidebotham, M., Gamble, J., Fenwick, J., & Creedy, D.
(2017). Factors influencing midwives’ use of an evidenced based Normal Birth
Guideline. Women and Birth, 30(5), 415–423. https://doi.org/10.1016/j.wombi.2017.03.008
Van Wagner, V. (2016). Risk talk : Using evidence
without increasing fear. Midwifery, 38, 21–28. https://doi.org/10.1016/j.midw.2016.04.009
Veeramah, V. (2016). The
use of evidenced-based information by nurses and midwives to inform practice. Journal of Clinical Nursing, 25(3–4), 340–350. https://doi.org/10.1111/jocn.13054
Appendix
Survey Instrument
- How many years have you been practicing as a
midwife?
·
0-40
- What is your highest degree earned?
·
Bachelors
·
Masters
·
PhD
·
Other
- Which province or territory do you practice in
predominantly?
- What is your status as Registered Midwife?
·
Full time
·
Part time
·
Non-practicing
·
Other
- Are you a midwifery
educator? (preceptor, NRP instructor, faculty position etc.)
·
Y/N
- In what setting are you
currently practicing? Select the best answer.
·
Urban
·
Suburban
·
Rural
·
Remote
- How often do you refer
to clinically-relevant, external information in the practice of midwifery?
(guidelines, manuals, books, websites)? 6-point Very frequently – Never
- Do you hold membership
in an academic library or hospital library? (Check all that apply)
·
Yes, through an academic library at a university where
I am faculty/employed/studying
·
Yes, through membership in a College or private
library (e.g. CMA, CFPC, CNA)
·
Yes, through my hospital (privileges/staff)
·
No, I do not hold membership in an academic/hospital
library
·
Unsure
·
Other
- If you answered Yes to
the above, how often do you access clinically-relevant information through
your academic or hospital library membership? (7 point Very frequently –
Never, N/A)
- How often do you visit
your local public library to find clinically-relevant information for
midwifery practice? (6 point Very frequently – Never)
- Please rank use of the following information
sources and modes of delivery in your midwifery practice:
·
Manuals (NRP, ALARM)
·
Colleagues
·
Studies (primary studies)
·
Popular websites
·
Print books
·
Social media
·
Summaries (clinical practice guidelines, systematic
reviews, algorithms)
·
Textbook-like e-resources (UptoDate,
DynaMed)
·
Apps
- Please rank the
challenges to using clinically relevant research in your practice
·
Lack of information access
·
Difficulty in judging the quality of the research
evidence
·
Difficulty relating research evidence to clinical
practice
·
Difficulty understanding statistical terms or jargon
·
Lack of skills in using specialized search tools
- The Association of
College and Research Libraries (2016) recognizes that information sources
must be evaluated “to acknowledge biases that privilege some sources of
authority over others, especially in terms of others’ worldviews, gender,
sexual orientation, and cultural orientations.” How relevant do you think
this statement is to the practice of midwifery? (5 point Very relevant –
Completely Irrelevant)
- Sackett et al. (2000)
describe evidence-based medicine as “the integration of best research
evidence with clinical expertise and patient values.” Based on this
statement how do you rate your competence in the following: (5-point
Expert – Novice)
·
Converting the need for information (about prevention,
therapy, diagnosis) into an answerable question
·
Tracking down the best evidence with which to answer
that question
·
Critically appraising that evidence for its validity
(closeness to truth) and usefulness (clinical applicability)
·
Applying evidence to the context of professional
practice
- Have you ever received
library skills training (i.e., Boolean operators, truncation, controlled
vocabularies, databases)? Check all that apply:
·
Yes, during my midwifery education and training
·
Yes, through my hospital or place of work
·
Yes, during the acquisition of a post-midwifery credential
·
No or cannot remember
·
Other (please elaborate)
- How interested would
you be in receiving library skills instruction relevant to midwifery?
(5-point Very Interested – Uninterested)
- Would you like to share
more detail about any of the above questions?